With perimenopause and menopause you experience complex shifts beyond estrogen and progesterone that reshape your hormonal ecosystem and influence sleep, mood, metabolism and bone health, so understanding these interactions lets you make targeted decisions about symptom management and long-term wellbeing.
The Hormonal Symphony: How Each Player Contributes
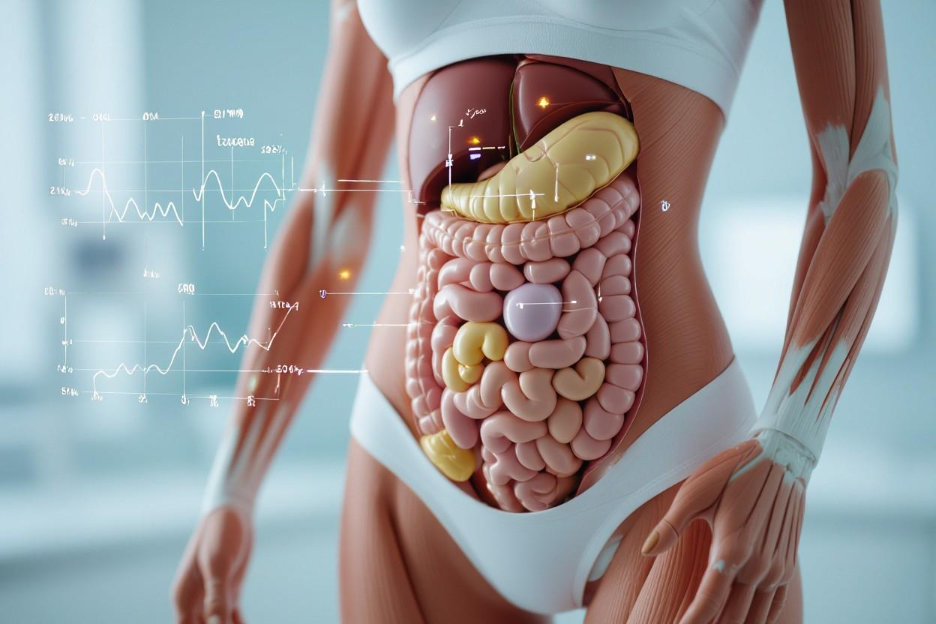
Think of your endocrine system as an orchestra: ovarian estrogen and progesterone are lead instruments, but adrenals, thyroid, pituitary and metabolic hormones provide rhythm and harmony. During perimenopause their relative volumes shift—FSH rises into the double digits (commonly >30–40 IU/L), estrogen production falls dramatically, and you may notice changes in sleep, bone density (1–2% loss per year early on) and mood as the ensemble retunes.
The Roles of Estrogen and Progesterone
Estrogen decline—often a 60–80% reduction from peak reproductive levels—drives hot flashes, vaginal dryness, and accelerated bone loss, while progesterone falls earlier because of anovulatory cycles, undermining sleep quality and mood stability. You may see cycle irregularity months to years before menopause as progesterone becomes intermittent and fluctuating estrogen produces symptoms that come and go, complicating diagnosis and management.
The Impact of Testosterone and Other Hormones
Testosterone decreases more slowly—total levels may drop roughly 30% across midlife—affecting libido, muscle mass, and vitality, while thyroid shifts and elevated cortisol alter metabolism and stress responses; these changes can increase central adiposity and impair recovery. You might notice reduced strength, lower exercise tolerance, and altered fat distribution as androgens and catabolic hormones rebalance.
Clinically, low testosterone links to measurable declines in lean mass and sexual desire: studies report notable muscle loss and strength reduction within five years postmenopause unless countered by resistance training or targeted therapy. Evaluation typically measures total/free testosterone, SHBG, TSH and morning cortisol to parse ovarian, adrenal or thyroid causes, guiding options like lifestyle intervention, thyroid correction, or selective hormone treatments where indicated.
The Perimenopausal Shift: What to Expect
You may first notice cycle changes in your early 40s as hormone output becomes irregular; the phase averages four years but can last up to a decade. Estrogen oscillations, falling progesterone and rising FSH ripple through sleep, metabolism, bone turnover and cardiovascular markers. About 75% experience symptoms like night sweats or mood shifts, and measurable bone loss (~1–2% annually after menopause) or altered lipids can emerge during this window.
Signs and Symptoms Beyond Hot Flashes
Irregular bleeding, heavier or lighter flow, and unpredictable cycles often precede menopause; roughly 40–60% report sleep disruption and night sweats. You may get vaginal dryness, urinary urgency, joint aches and central weight gain—especially increased abdominal fat. Libido changes and hair thinning are common; tracking symptoms and cycles for 6–12 months helps clarify patterns and guide treatment decisions.
Emotional and Cognitive Changes During Transition
You may notice mood swings, heightened anxiety or low mood—studies show up to 20% experience significant depressive symptoms during perimenopause. Concentration lapses, word-finding trouble and short-term memory slips are frequent as estrogen fluctuations affect hippocampal and prefrontal circuits that support memory and executive function. Documenting timing alongside menstrual changes helps distinguish hormonal effects from other causes.
Poor sleep and night sweats often amplify cognitive and emotional complaints, so improving sleep and treating vasomotor symptoms can produce measurable gains. Cognitive-behavioral therapy and regular exercise (about 150 minutes/week) lower anxiety and depressive scores; SSRIs or SNRIs are effective for clinically significant mood disorders, and menopausal hormone therapy started near menopause may ease mood and memory issues for some. Discuss risks, benefits and timing with your clinician, and consider neurocognitive testing if symptoms disrupt work or daily life.
Menopause Unveiled: Navigating the New Normal
You may notice shifts beyond periods stopping: sleep fragmentation, hot flashes, vaginal dryness, and changes in mood and cognition. Average U.S. menopause age is 51, with vasomotor symptoms affecting roughly 50–75% of women; metabolic shifts favor central fat gain and reduced insulin sensitivity. Practical adjustments—targeted exercise, sleep strategies, pelvic health care, and medical review—help stabilize daily function.
Biological Changes and Their Impacts
As ovarian estrogen and progesterone fall, you experience systemic ripple effects: bone turnover increases (early postmenopause bone density loss can be ~1–2% per year), LDL cholesterol and blood pressure often rise, and insulin resistance can worsen. Adrenal androgens play a relatively larger role, sometimes preserving libido, while disrupted sleep and memory complaints directly reflect these hormonal cascades.
Long-term Health Considerations and Risks
Long-term, you face higher risks of osteoporosis and fractures—your lifetime risk of an osteoporotic fracture can approach 40%—and rising cardiovascular disease risk as protective estrogen wanes. Incidence of metabolic syndrome increases, elevating diabetes and stroke likelihood. Untreated bone loss and uncontrolled lipids contribute to morbidity decades after menopause, so proactive risk assessment matters.
Screening and prevention change outcomes: obtain a DEXA scan by age 65 (earlier with risk factors), aim for roughly 1,200 mg calcium and 800–2,000 IU vitamin D daily, and do weight-bearing exercise 3–4 times weekly. Discuss hormone therapy within about 10 years of menopause or before ~60 for symptom relief and bone benefit, assess ASCVD risk for statin use, and prioritize smoking cessation and alcohol moderation to lower long-term harm.
The Ripple Effect: Hormones and Your Overall Wellbeing
Hormonal shifts during perimenopause and menopause ripple through thyroid, cortisol, insulin and adrenal axes, altering metabolism, sleep, immunity and bone health. You may notice slowed metabolism, increased central fat and shifts in cholesterol; menopause typically occurs around age 51 and perimenopause can last up to 10 years. Fluctuating estrogen also impairs bone remodeling by reducing osteoblast activity, raising fracture risk without targeted prevention.
Hormonal Interactions with Mental Health
Estrogen and progesterone modulate serotonin, GABA and norepinephrine pathways, so you can experience mood swings, anxiety or brain fog as levels change. Night sweats and fragmented sleep amplify emotional symptoms; one longitudinal study found women in early menopause reported roughly twice the rate of depressive symptoms versus premenopausal peers. Screening for new or worsening depression during transitions helps guide timely treatment decisions.
Lifestyle Strategies for Balancing Hormones
Targeted lifestyle changes stabilize many hormonal effects: aim for 150 minutes of moderate aerobic activity weekly plus two strength sessions to protect bone and muscle; consume 1.0–1.2 g protein/kg daily, 1,200 mg calcium and 800–1,000 IU vitamin D, and add about 1 g EPA+DHA omega3 for mood support. Prioritize sleep hygiene, reduce refined carbs and limit alcohol to lower vasomotor symptoms and insulin spikes.
Create a practical weekly plan: three 30minute brisk walks and two 45minute resistance sessions, plus a 10–20 minute daily mindfulness practice to blunt cortisol surges. Try breakfasts like Greek yogurt with berries and 20–30 g protein, include fatty fish twice weekly, and use a 2week symptom diary to track sleep, hot flashes and mood. Request baseline labs (TSH, fasting glucose, lipids, 25OH vitamin D, and FSH if symptomatic) to tailor interventions and discuss HRT or other medical options with your clinician.
Reframing the Narrative: Embracing Change and Empowerment
You can approach this phase as a deliberate recalibration: track symptoms, prioritize interventions, and set new health goals rather than viewing changes as decline. Perimenopause typically spans about four years and menopause averages near 51, so targeted steps—like structured exercise, sleep optimization, and evidence-based therapies—can restore function; menopausal hormone therapy relieves vasomotor symptoms for roughly 70–75% of users, illustrating how informed choices translate into regained control and daily improvements.
Societal Perceptions of Aging and Womanhood
Cultural narratives still prize youth, which leaves many women feeling invisible even though up to 75–85% experience menopausal symptoms such as hot flashes or sleep disruption. You confront both physical transition and social bias: workplace stigma, marketing that excludes midlife bodies, and lack of clinician training magnify distress. Concrete shifts—visibility in media, workplace menopause policies, and age-inclusive product design—help counteract these pressures and validate your lived experience.
Tools and Resources for Support and Education
Turn to vetted organizations (North American Menopause Society, National Institute on Aging, national health services) for guidelines, and seek multidisciplinary care—gynecologists, menopause-trained internists, menopause nurse specialists, dietitians, pelvic-floor physiotherapists, and CBT therapists—for symptom-specific strategies. Utilize symptom trackers, accredited online courses, peer support groups, and employer resources; telehealth expands access so you can combine local clinicians with national guideline-based care.
Practical next steps: document symptom frequency and severity for 4–12 weeks, ask clinicians about benefits/risks of HRT (noting ~70–75% efficacy for hot flashes), discuss nonhormonal options if indicated, and request referrals to CBT for insomnia or anxiety, pelvic-floor therapy for genitourinary symptoms, and nutrition counseling for bone and metabolic health. Use decision aids from professional societies, verify clinician menopause training, and join local or online support groups to compare real-world strategies and timelines.
Summing up
Following this overview, you can see that perimenopause and menopause reshape more than estrogen and progesterone; they alter your thyroid, adrenal, insulin, and neurohormone balance, influencing mood, sleep, metabolism, and bone health. With targeted monitoring and interventions you can manage symptoms, support resilience, and maintain long-term wellbeing.